NICU PATIENT CARE FOR YOUR 1:1 ASSIGNMENT
Some patients are so medically complex, unstable, and incredibly fragile that they cannot safely be paired with another baby. This means that one nurse is responsible for one baby ONLY. That said, oftentimes these babies are the absolute smallest ones on the unit and require care tasks that take up every second of your 12-hour shift. The nurse may not even have time to sit down and chart or take a break until the late afternoon. If you were caring for a very high acuity 1-to-1 patient, here is a rundown of what a typical shift may look like for you:
Sample diagnoses that may require 1:1 care:
ECMO
Pre-op Cardiac Surgery
Unstable vent (Jet, High Frequency Oscillator, VDR4, etc.)
Hypothermia therapy
Micropreemies
Pre/Post-Op Surgical patients
Complex chronic lungers
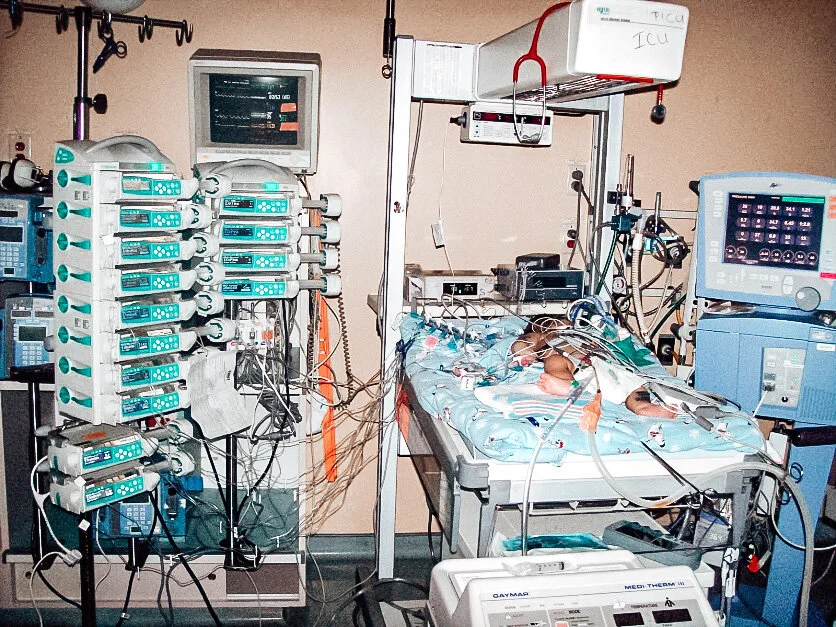
Let’s say that the nurse is caring for a baby that was born at 23 weeks gestation. The bed area is most likely going to have the following equipment:
A High Frequency Oscillating Ventilator (these things are BEASTS but are SO gentle on the lungs)
Multiple IV pumps + poles with a variety of medications running
A cardiopulmonary monitor displaying heart rate, oxygen saturation, and respiratory rate
An isolette with humidity
Possibly a Bili-light used to assist the body in breaking down bilirubin (increased levels cause jaundice).
0700
After scrubbing in and removing all jewelry per your NICU’s policy, you will start your report around 7:00 (AM or PM). Report typically finishes around 7:30 (AM or PM), and shortly after that you would begin your first round of care on the infant. After assessing the safety of the bedside (i.e. ensuring your suction works, your bag & mask inflates, and visualizing your emergency drug sheet), you would start your shift by sanitizing the bedspace and everything that you plan on touching throughout the day at your baby’s bedside. Remember: you are working in the ICU, and this patient population is extremely susceptible to getting sick and acquiring infections. Wiping down all of the high-touch areas (isolette, IV pumps, stethoscope, work area, charting area, work phone, etc.) is so important to prevent the spread of germs and bacteria.
Next, you would double check your orders, assess your lines, drains, & airways, and touch base with your respiratory therapist (RT) to come up with a game plan for the day. More than likely, your patient is considered to be “minimal handling” (AKA min stim) meaning you will perform cares every 6 hours (twice a shift) in order to promote sleep, reduce hypothermia & hypoglycemia, and decrease the risk of intraventricular hemorrhage (IVH), bronchopulmonary dysplasia (BPD), and retinopathy of prematurity (ROP).
For example, your “touch times” would probably be 0800/2000 hours and 1400/0200 hours. You will group or “cluster” your cares with the RT in order to minimize disrupting your baby’s sleep. On the off hours, only monitor vitals are obtained to allow the patient a chance of having a period of uninterrupted sleep. Of course, all of this is dependent on the acuity of the patient, vitals may be needed more often, or the RN may be disturbing the infant more frequently in order to keep the patient safe and alive.
0800
After devising a game plan for the shift (i.e. what times you and the RT are going to perform your cares simultaneously), you would gather all of the supplies that you need so that you’re ready to go. Your first round of cares will include a head-to-toe assessment, diaper change, temperature check, pulse check, eye care, and so much more. It is important to be thorough but also quick in order to save time, decrease heat loss (since the isolette doors will be open for a period of time) and provide containment to foster proper development. For example, while auscultating and counting the heart rate and respiratory rate, I am working on my head to toe assessment. While feeling the fontanelles, I am performing a neuro check. And while obtaining my girth, I am assessing abdominal quality and checking residual.
When reviewing orders in the morning, if there was a scheduled chest x-ray at 0800 and labs to draw, I would time these tasks together. If my OG tube was due to be changed at a certain time, I would wait to perform my cares until that point in order to minimize disturbances. In addition, most procedures are done at the bedside in the NICU: PICC line placement, lumbar punctures, ultrasounds, to name a few. So I would work my day around the time that these procedures are ordered, or I would schedule these procedures during my “touch” times. I would also let my doctor know when we are doing touch time so he/she can examine the baby during this time as well.
After obtaining blood pressure measurements (with the tiniest blood pressure cuff you have ever seen!) and an axillary temperature, I work on several other checks from head to toe. I perform oral hygiene with any colostrum that we may have available from mom, check the OG tube to remove any air from the stomach, suction out the ET tube and make mental note of the secretions, and lastly change the infant’s diaper. Diapers are weighed from admission to discharge in order to measure intake and output.
If you performed a morning blood gas, and chest x-ray, this may or may not have resulted in some ventilator setting changes. As the bedside nurse, you are actively managing the patient’s oxygen concentration to keep their saturations between the ordered parameters. Too much oxygen for too long can be detrimental to the infant’s developing retinas, and too low is starving the body of the needed oxygen.
Bedside rounds (0900)
Depending on the facility, the neonatologist may round on your baby by himself/herself OR with the entire interdisciplinary care team. If all specialties (MD, bedside RN, RT, PT, OT, ST, SW, case manager, charge nurse, pharmacist, dietitian, etc.) present to the bedside, they will collectively discuss the plan of care and changes that need to be made to the neonate’s daily needs. Then, the doctor will explain this to the parents if they are present at the bedside. If not, they will try to contact them by phone for a daily update. After the plan of care for the day is discussed, you won’t change anything until your orders are written.
1000
Around 1000, charting begins! Every hour, monitor vitals, isolette temperatures, and IV pump rates + volumes must be recorded and documented. Some babies may be on one, two, three, IV drip medications that should be titrated based on monitor data (e.g. dopamine, morphine, etc.) and may require more frequent charting (Q15 minutes, for example). It is practice in my unit to obtain hourly vitals including heart rate, respirations, pain scores, oxygen saturation, and arterial BP (if your baby has umbilical lines).
As the bedside RN for a critically ill or premature infant, you really are not ever leaving that bedside. You will be constantly and closely watching the patient’s vital signs, reporting changes in status to the neonatologist, explaining changes to the parents, and charting EVERYTHING. When it’s time for you to take your break, another nurse will cover your assignment and watch your baby.
If your baby is “stable” enough to be held, another job of yours is assisting parents with kangaroo care. NICU nurses promote family-centered care and encourage family involvement when performing care tasks. This includes teaching parents how to change a diaper, educating them about your assessment findings and if anything has deviated from the baby’s baseline, helping them with feeding techniques, and providing information about pumping and breast milk.
In addition, product transfusions (PRBCs, FFP, Platelets, exchange transfusions), administering medications, starting new IVs (with a 24 gauge catheter), drawing labs, or requesting assistance with repositioning your patient may occur several times throughout your shift.
By now, it’s probably your next “touch” time, and you will do everything that you did in the morning all over again!
It is on days like this when your brain is working in overdrive and going a million miles an hour. All of your critical thinking skills are used and abused. It is such a rush in the beginning of the shift which then transitions to alarm fatigue from the loud noise of the ventilators and the monitors and pumps constantly beeping. I come home on these days and everything hurts: my brain, eyes, feet, and bladder. My ankles are swollen, and it takes everything in me to muster up the energy to shower, pack my lunch for the next day, and then wake up and do it all over again.